Artificial Intelligence in Healthcare: Real Revolution or Overheated Hype?
29.11.24 | Michaela Ziegler
In healthcare, expectations for AI are high. From automated diagnoses to personalized treatment plans, many see AI as the key to revolutionizing medicine.
I am doubly interested in this topic. On one hand, I’m a consumer with an AI-powered fitness watch that tells me (optimistically) I can run a marathon in under four hours. On the other, I’m a digital health consultant who hopes that AI will help us extract more structured data from the Swiss Electronic Patient Record (EPR).
So I asked myself: Is AI really that revolutionary? Or are we expecting too much on another over-hyped technology.
With this question in mind, I went to Berlin this summer to complete a course at the Institute for Communication and Leadership (IKF) called CAS Healthcare Transformation — With AI to more intelligence in healthcare. I gained many new and exciting insights into the current status and potential of AI in healthcare, which have sharpened my view of the possibilities (and the limitations) of the technology. In this post, I want to share the most important lessons I brought back from Berlin.
Before that, some definitions and some history might be helpful. Let’s take a brief look at how AI is defined and what it involves.
AI at a glance: Definitions and demarcations
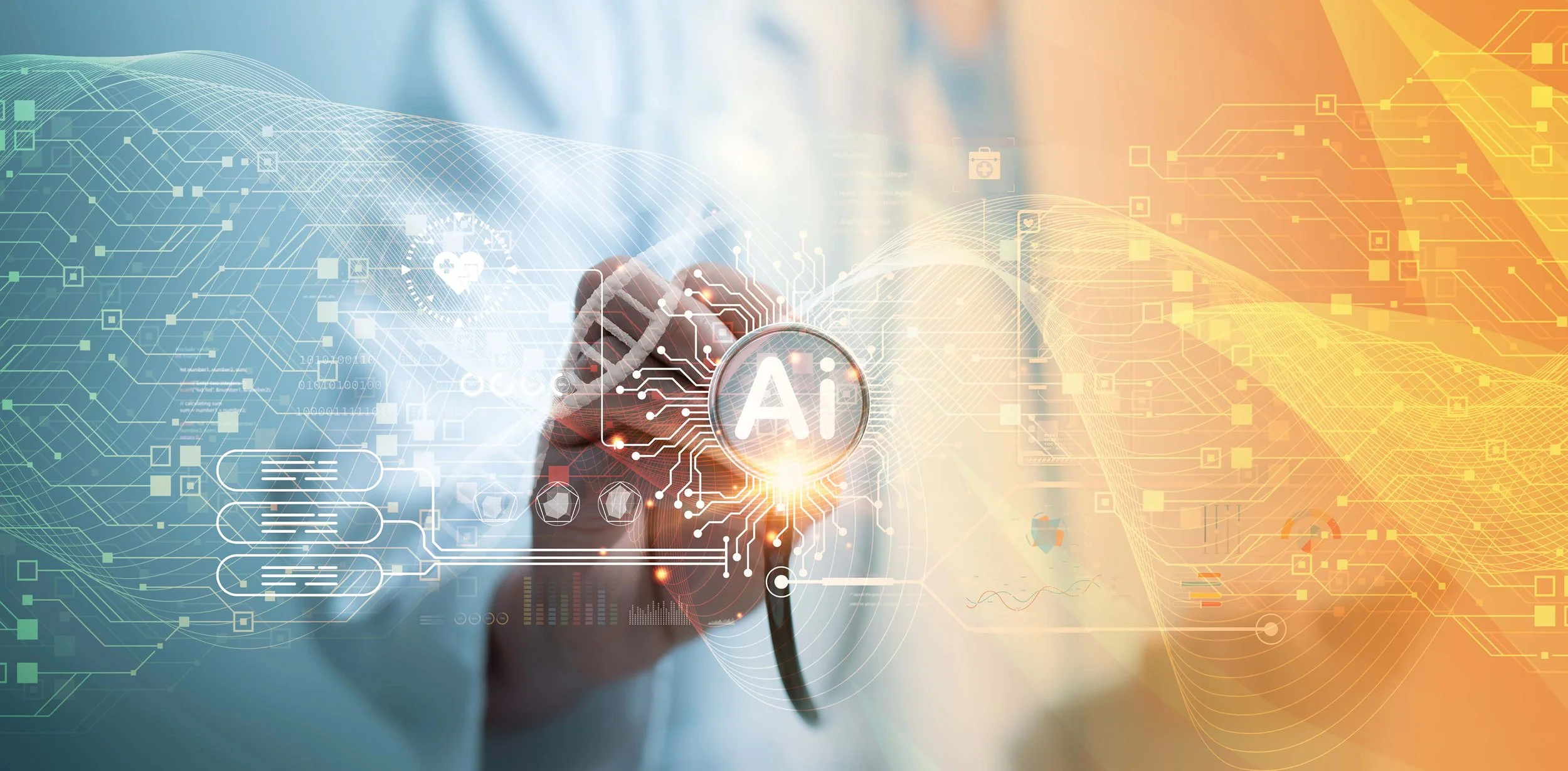
Artificial intelligence refers to the ability of machines to perform human-like cognitive functions, such as learning, problem solving and decision making. It’s a broad field that has developed over several decades and encompasses various techniques, with more traditional AI models being based on predefined rules and data sets.
Generative AI (GenAI) is a more recent development. As the name suggests, GenAI generates new content — text, audio, images or videos — and can be seen as part of the wider concept of ‘deep learning’.
Fig. 1: The development and specialization of AI from the 1950s to today.
GenAI has come to public attention through popular large language models (LLMs) like ChatGPT. Unlike the more traditional models, LLMs like ChatGPT are trained on large, diverse data sets to build up a broad base of what looks like knowledge.
However, GenAI doesn’t actually know anything. Its outputs are based instead on predictions and probabilities. One of the challenges of GenAI, therefore, is the phenomenon of hallucinations — or content that appears realistic but deviates from the given source inputs. This lack of faithfulness or factualness complicates both the reliability of the models and their practical application.
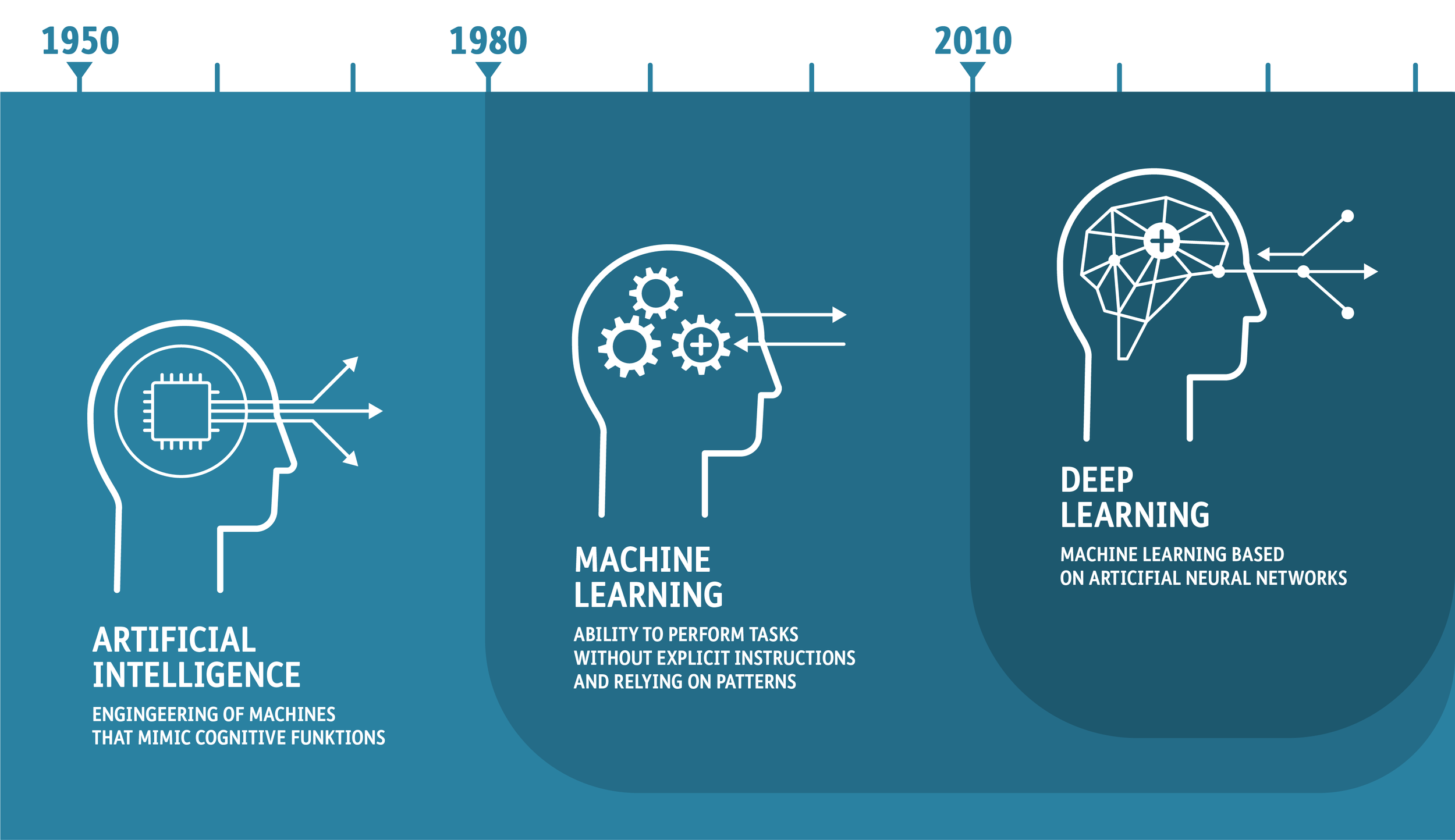
The following is a classic test of ChatGPT:
Fig. 2: An example of AI hallucination: A simple question with an unexpected answer.
The answer sounds reasonable but is objectively false. This is because ChatGPT cannot distinguish between actual truth and the probability of something being true.
In healthcare, AI models can be used in different ways. LLMs can perform a variety of tasks from communicating with patients to analyzing medical texts and assisting with diagnoses. In contrast, specialized models with a narrower focus on specific applications can play a decisive role in image analysis or the processing of genetic data.
So, the first take-home messages in my ‘Berlin suitcase’ are:
• Any constructive discussion of AI in healthcare has to be clear about which area of AI is being considered, especially when talking to non-experts. Consider weather forecasting as an example. If you want to go skiing at the weekend, you would use an app that uses meteorological models to predict weather conditions. You wouldn’t trust your weekend plans to ChatGPT.
• Hallucinations have become a huge focus in current AI development. People are looking at which approaches are suitable for minimizing the risk of hallucinations.
• LLMs and specialized models should be used strategically as needed to ensure both efficiency and accuracy.
The state of AI in healthcare: Possible applications and challenges
The implementation of AI in the healthcare sector is at different stages in different areas. For example, it is already proving to be a valuable tool in medical research. Studies show that AI-supported systems are able to recognize patterns and anomalies in large data sets that would be difficult for human experts to identify. In radiology, for example, AI models can improve the accuracy of diagnoses by analyzing images faster and more precisely than humans. Genomics is another area in which AI offers great opportunities.
However, widespread adoption in everyday clinical practice has fallen short of expectations. There are numerous potential applications for AI in clinical medicine, from diagnostics to personalized therapy. But many of these technologies struggle with the challenges of actual implementation in practice, and many healthcare facilities are reluctant to integrate AI solutions.
A key obstacle is the regulatory requirements placed on AI applications in the healthcare sector. These regulations are there to ensure the safety and effectiveness of AI-supported tools, but can also inhibit the innovation process. Approval procedures are often lengthy and require extensive proof of system performance and safety.
Data protection is just as important. Sensitive health data is naturally subject to strict legal requirements. The fear of data misuse and breaches makes many organizations reluctant to implement AI-supported solutions.
Low user acceptance is also critical. Many healthcare professionals are skeptical about AI, and are concerned about the reliability of AI systems and worried about losing their decision-making autonomy. Clearly communications about the advantages and benefits of AI in daily practice are needed to overcome these hurdles.
The second take-home messages in my Berlin suitcase are, therefore:
• AI’s hurdles in healthcare are familiar: regulations and data protection. We have seen these before. You should get involved early on and communicate well, but don't lose heart.
• Communicating concrete benefits will help increase acceptance of AI. An example from the field of nursing: AI-powered medication checks increase patient safety and reduce (mental) stress for nursing staff.
Humans and AI as a team: From a product-centric to a human-centric approach
To promote acceptance of AI in healthcare, we need to make the technology comprehensible. Black-box models for example have known inputs and outputs but opaque decision-making processes that users barely understand. In contrast, white-box models openly present their logic and decision-making process – which is why they are also known as explainable AI (XAI). This transparency enables traceability, human interaction, and validation by experts. The transition from black-box to white-box models allows users to see how and why decisions are made.
It also helps to add value compared to previous concepts. Consider AI-controlled prostheses. They are an impressive example that adapt to the individual needs of users, which means those users no longer have to learn standard programs to operate them. This is a paradigm shift away from a product-centric to a human-centric approach, and is essential for broader acceptance.
In effect, combining human expertise with AI technologies is the key to success. Although AI provides powerful data analytics and pattern recognition, human judgment is still needed to bring context and empathy to decision-making processes. Together, humans and machines play a central role in creating an effective and trustworthy healthcare system.
The third set of take-home messages in my Berlin suitcase are:
• Although new to me, the white-box model looks like a really important way to increase acceptance.
• AI-controlled hand prosthesis are amazing! The added-value compared to older model is so obvious: more grip and movement options, simpler control and, above all, the prosthesis learns from the person not the other way around. That puts the human being at the center. WOW!
Data as the basis for AI: From unstructured data to meaningful information
Structured data is the basis for effective AI solutions, as it allows more precise analysis and processing. Without a clear and uniform data structure, it will be hard to realize the full potential of AI.
The European Health Data Space (EHDS) could act as a game changer here by improving the use of data. By creating a common framework for health data within the EU, we can use existing data better, and open up new opportunities for innovative AI applications and ultimately research and patient care.
In Switzerland, the so-called ‘PDF graveyard’ of the Electronic Patient Record (EPR) is a much-cited problem. A lot of health data is currently only available in PDF format, which is unstructured. By using AI, we can convert it into structured information, which is then made available in interoperable and international formats such as HL7 FHIR. Conversion would enable better use of data, and close the loop in which AI contributes to the structuring of healthcare data and thus forms the basis for future-oriented applications in healthcare.
When converting unstructured data into structured formats we need to ensure correctness – so it’s an area where hallucinations are a challenge. A professional review should ensure that we receive reliable results before we use them in clinical practice. But who should carry out this evaluation? Is it the job of data scientists, healthcare professionals or another body to ensure quality control?
With this in mind, the final take-home messages in the Berlin suitcase are:
• Data is the key to success. And instead of grumbling about unstructured data, we should think about how we can use it sensibly to provide us with a basis for future solutions.
• Despite the potential for creating structured data sources, the quality of the results must always take precedence over quantity.
Vision: AI as the path to the healthcare system of tomorrow
I came back from Berlin, and back to my original question: Is AI revolution or hype?
In my view, AI has enormous potential for a human-centered healthcare system. It can help optimize processes, enable personalized treatments, and increase efficiency. One example of process optimization is AI-controlled image analysis in radiology, which makes diagnoses earlier and more precisely. Personalized treatments could be made possible by AI-based systems that create individually tailored treatment recommendations based on patient data.
AI can also support the automation of administrative tasks, such as the documentation of patient information, and so free up valuable time for direct patient care. At the same time, however, we must be careful with further development, and focus on the human-centered approach, high user acceptance through traceability, and the combination of human and artificial intelligence working together.
Ultimately, we should take a critical but open approach to the topic of AI in healthcare. It is up to us to seize the opportunities and overcome the challenges in order to shape a future in which AI can actually enrich our healthcare system.
I found Artificial intelligence (AI) in the Swiss healthcare system (in German), which was commissioned by the Federal Office of Public Health (FOPH) to be a valuable contribution. It is intended to serve as a basis for technical discussions and strategic decisions in order to shed light on the various areas of the Swiss healthcare ecosystem in relation to AI. Among other things, it examines how the opportunities of AI use can be exploited and risks minimized, the significance of introducing AI tools in areas like data protection, research and care, and how they can be scaled to offer real added value to both providers and patients.
As for our work at ahdis, an exciting example of the practical application of AI in healthcare is currently being discussed as part of a living case in the Medical Informatics course at Bern University of Applied Sciences (BFH) (term paper). Two students are evaluating how AI can be used to optimize our validation tool Matchbox. The AI should help to make the rather technically formulated error messages that are issued as output during validation with Matchbox more comprehensible. We are excited to see what impact AI will have on our open-source solution.
A final message from Berlin and a visual treat
I would like to pay a personal tribute to the AI in my fitness watch which went jogging with me in the Berlin Tiergarten: Dear AI, your optimism is inspiring, but we know each other better by now. You have recognized (or rather, my data has shown you) that I will probably need a little more than four hours for a marathon! 😉
Fig. 3: A photo from my morning tour of the Tiergarten. It is real, only the exposure has been slightly optimized by AI.